Blood and its Constituents.
Constituents and Functions of Blood.
• Blood: A specialized bodily fluid that delivers necessary substances to the body’s cells such as nutrients, oxygen and transports waste products away from those same cells
• Blood accounts for 7% of the human body weight
• By volume the red blood cells constitute about 45% of whole blood, the plasma constitutes about 55%
• The average adult has a blood volume of roughly 5 litres, composed of:
o Plasmao Formed elements
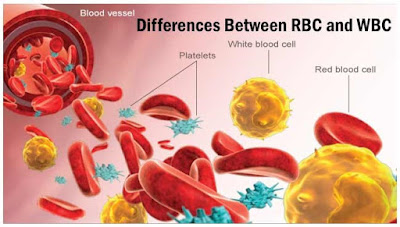
• These formed elements of the blood are
o Erythrocytes (red blood cells)o Adult humans have roughly 2–3 × 1013 red blood cellso Leukocytes (white blood cells) and 4,000–11,000 white blood cellso Thrombocytes (platelets). 150,000–400,000 platelets in each microliter
• Women have about 4 to 5 million erythrocytes per microliter (cubic millimeter) of blood and men about 5 to 6 million; people living at high altitudes with low oxygen tension will have more
Functions.
• Supply of oxygen to tissues (bound to haemoglobin which is carried in red cells)
• Supply of nutrients such as glucose, amino acids and fatty acids (dissolved in the blood or bound to plasma proteins (e.g. blood lipids)
• Removal of waste such as carbon dioxide, urea and lactic acid
• Immunological functions, including circulation of white cells, and detection of foreign material by antibodies
• Coagulation, which is one part of the body’s self-repair mechanism
• Messenger functions, including the transport of hormones and the signalling of tissue damage
• Regulation of body pH (the normal pH of blood is in the range of 7.35 – 7.45)
• Regulation of core body temperature
Blood Plasma.
• The fluid portion of the blood, the plasma, is a remarkable solution containing an immense number of ions, inorganic molecules, and organic molecules that are in transit to various parts of the body or aid in the transport of other substances.
• The normal plasma volume is about 5% of body weight, or roughly 3500 mL in a 70kg man.
• Plasma clots on standing, remain fluid only if an anticoagulant is added.
• If whole blood is allowed to clot and the clot is removed, the remaining fluid is called serum.
• Serum has essentially the same composition as plasma except that its fibrinogen and clotting factors II, V, and VIII have been removed and it has higher serotonin content because of the breakdown of platelets during clotting.
• The plasma consist of protein; albumin, globulin, and fibrinogen fractions.
• The capillary walls are relatively impermeable to the proteins plasma, and the proteins are therefore exerting an osmotic force of about 25 mm Hg across the capillary wall (oncotic pressure) that pulls water into the blood.
• The plasma proteins are also responsible for 15% of the buffering capacity of the blood because of the weak ionization of their substituent COOH and NH2 groups.
• At the normal plasma pH of 7.40, the proteins are mostly in the anionic form and constitute a significant part of the anionic complement of plasma.
• Plasma proteins such as antibodies and the proteins concerned with blood clotting have specific functions.
• Most of the other plasma proteins are synthesized in the liver.
Production and Functions of Red Blood Cell.
Red Blood Cells Formation.
• The cells are filled with hemoglobin, a biomolecule that can bind to oxygen.
• They take up oxygen in the lungs and release it while squeezing through the body’s capillaries.
• The blood’s red colour is due to the colour of hemoglobin.
• In humans, red blood cells develop in the bone marrow, take the form of flexible biconcave disks, lack a cell nucleus, subcellular organelles and the ability to synthesize protein, it takes about 7 days for erythrocytes to mature and live a total of about 120 days.
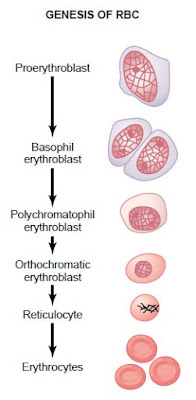
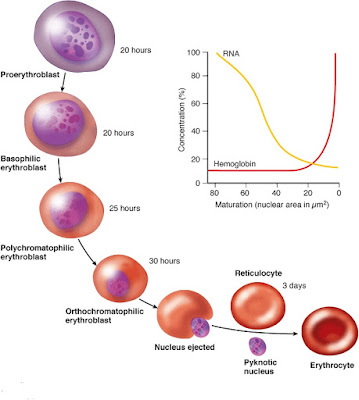
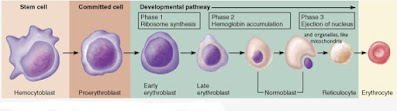
o Erythropoiesis is the process by which red blood cells (erythrocytes) are produced.o In human adults, this usually occurs within the bone marrow.o In the early fetus, erythropoiesis takes place in the mesodermal cells of the yolk sac.o By the third or fourth month, erythropoiesis moves to the spleen and liver.o In humans with certain diseases, erythropoiesis also occurs outside the bone marrow, within the spleen or liver.o This is termed extramedullary erythropoiesis.o The tibia and femur cease to be important sites of hematopoiesis by about age 25; the vertebrae, sternum, pelvis and ribs, and cranium bones continue to produce red blood cells throughout life.o Erythrocytes and granulocytes belong to the myeloid lineage.o The earliest identifiable erythroid stem cells are capable of rapid bursts of cell division to form numerous daughter cells.o In the process of red blood cell maturation, a cell undergoes a series of differentiations.o The following stages of development all occur within the bone marrow.o Pluripotent haematopoietic stem cell is cells which are capable of giving rise to all blood cell types.o The first readily identifiable cell of the erythroid series is the proerythroblast, a large cell with a large euchromatic nucleus and moderately basophilic cytoplasm.o It also responds to erythropoietin.
o The proerythroblast contains small amounts of ferritin and bears some of the protein spectrin on its plasma membrane.
o Proerythroblasts proliferate to produce smaller basophilic erythroblasts, rich in ribosomes, in which haemoglobin-RNA synthesis begins.o The cytoplasm becomes partially, and then uniformly, eosinophilic (the polychromatic erythroblast and orthochromatic erythroblast respectively).o The nucleus becomes intensely pyknotic and is finally extruded from the cell, leaving an anucleate reticulocyte, which enters a sinusoid.o Its reticular staining pattern, visible using special stains, results from residual cytoplasmic RNA which is lost within 24 hours of entering the peripheral blood circulation.o Reticulocyte numbers in peripheral blood are therefore a good indicator of the rate of red cell production.o The whole process of erythropoiesis takes 5-9 days.
Regulation of Erythropoiesis.
• Erythropoietin (EPO) is a glycoprotein (protein-sugar conjugate) that serves as the primary regulator of red blood cells (erythrocytes).
• It stimulates bone marrow stem cells to differentiate into red blood cells and controls haemoglobin synthesis and red blood cell concentration.
• EPO production is stimulated by reduced oxygen content in arterial blood in the kidneys.
• Circulating EPO binds to receptors on the surface of erythroid progenitor cells that in turn mature into red blood cells.
• In infants, EPO is produced mostly in the liver, but the kidneys become the primary site of EPO synthesis shortly after birth.
Production and Function of White Blood Cells.
• White blood cells, or leukocytes, are cells of the immune system defending the body against both infectious disease and foreign materials.
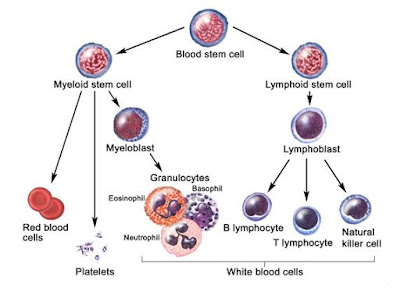
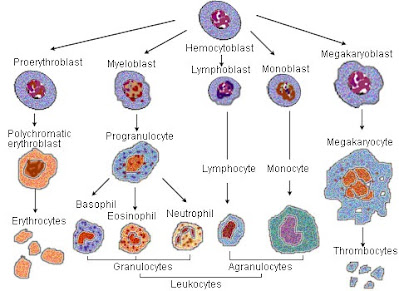
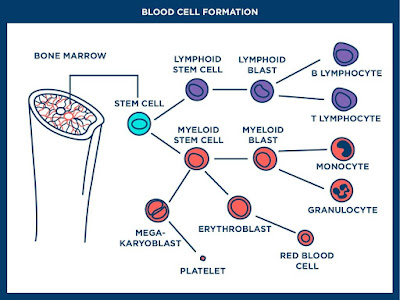
• Five different and diverse types of leukocytes exist, but they are all produced and derived from a multipotent cell in the bone marrow known as a hematopoietic stem cell.
• Leukocytes are found throughout the body, including the blood and lymphatic system.
• The number of leukocytes in the blood is often an indicator of disease.
• There are normally between 4×109 and 11×109 white blood cells in a litre of blood, making up approximately 1% of blood in a healthy adult.
• In conditions such as leukemia, the number of leukocytes is higher than normal, and in leukopenia, this number is much lower.
Types of White Blood Cells.
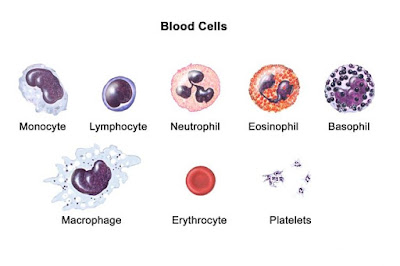
• There are several different types of white blood cells.
• They all have many things in common, but are all different.
• One primary technique to classify them is to look for the presence of granules, which allows the differentiation of cells into the categories granulocytes and agranulocytes
Granulocytes (Polymorphonuclear Leukocytes).
• Leukocytes characterised by the presence of differently staining granules in their cytoplasm when viewed under light microscopy.
• These granules are membrane-bound enzymes which primarily act in the digestion of endocytosed particles.
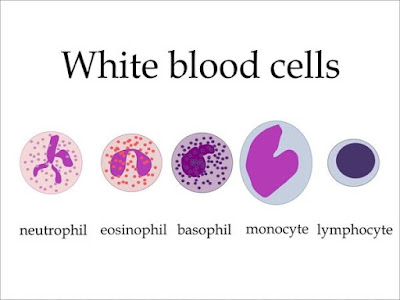
• There are three types of granulocytes: neutrophils, basophils, and eosinophils, which are named according to their staining properties.
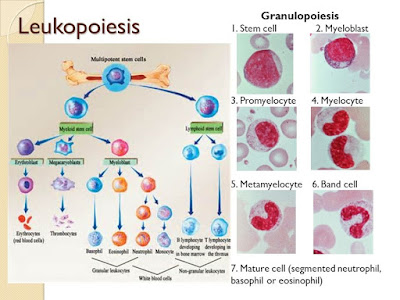
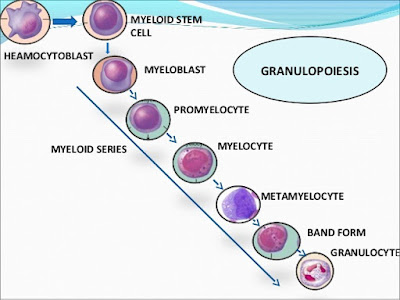
• Granulocyte formation involves major changes in nuclear morphology and cytoplasmic contents which are best known for the neutrophil.
• Initially, myeloid stem cells transform into large myeloblasts which are similar in general size and appearance to proerythroblasts.
• These proliferative cells have large euchromatic nuclei and lack cytoplasmic granules.
• They differentiate into slightly larger promyelocytes, in which the first group of specific proteins is synthesized in the rough endoplasmic reticulum and Golgi apparatus.
The proteins are stored in large primary (non-specific) granules, which are large lysosomes containing acid phosphatase.
• Smaller secondary (specific) granules are formed in the smaller myelocyte, which is the last proliferative stage.
• The nucleus is typically flattened or slightly indented on one side in myelocytes.
• In metamyelocyte, stage, the cell size decreases, the nucleus becomes heterochromatic and horse-shoe shaped, and protein synthesis almost stops.
• As the neutrophil is released, the nucleus becomes first heavily indented and subsequently segmented into up to six lobes, characteristic of the mature neutrophil.
• The whole process takes 7 days to complete, of which 3 days spent proliferating, and 4 days are maturing.
• Neutrophils may then be stored in the marrow for a further 4 days, depending on demand, before their final release into the circulation.
• Eosinophils and basophils pass through a similar sequence but their nuclei do not become as irregular as that of the neutrophil.
• Basophils nucleus is bi- or tri-lobed, but it is hard to see because of the number of coarse granules which hide it.
• They are characterised by their large blue granules.
• Eosinophils nucleus is bi-lobed.
• The cytoplasm is full of granules which assume a characteristic pink-orange color with eosin stain.
• Neutrophils are also known as polymorphonuclear leukocytes.
• They have a multilobed nucleus which may appear like multiple nuclei, hence the name polymorphonuclear leukocyte.
• The cytoplasm may look transparent because of fine granules that are faintly pink in color.
Agranulocytes (Mononuclear Leucocytes).
• Leukocytes characterized by the apparent absence of granules in their cytoplasm.
• Although the name implies a lack of granules these cells do contain non-specific azurophilic granules, which are lysosomes.
• The cells include monocytes, macrophages and lymphocytes.
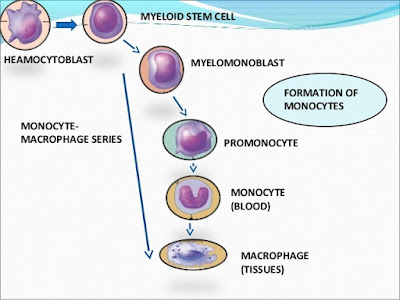
• Monocyte progenitors pass through a proliferative monoblast stage.
• A typical monoblast is about 12 to 20 μm in diameter, has a round to oval nucleus with fine chromatin structure.
• The nucleus can be central or eccentric and it can show evidence of indentation or folding.
• The cytoplasm is agranular, stains moderately to lightly basophilic, and often has an intensely stained periphery and a prominent perinuclear zone.
• Monoblasts are normally found in bone marrow and do not appear in the normal peripheral blood.
• They mature into monocytes which in turn develop into macrophages.
• The monoblast is the first stage of monocyte-macrophage maturation.
• The developmental stages of the monoblast are
o Pluripotential Hemopoietic Stem Cell or hemocytoblasto Monoblasto Promonocyteo Monocyteo Macrophage
• Lymphoblasts are normally found in the bone marrow, but in acute lymphoblastic leukaemia (ALL), lymphoblasts proliferate uncontrollably and are found in large numbers in the peripheral blood.
Functions of White Blood Cells.
Neutrophil.
• Neutrophils defend against bacterial or fungal infection and other very small inflammatory processes that are usually first responders to microbial infection; their activity and death in large numbers forms pus.
• Neutrophils are very active in phagocytosing bacteria and are present in large amount in the pus of wounds.
• These cells are not able to renew their lysosomes used in digesting microbes and die after having phagocytosed a few pathogens
Eosinophil.
• Eosinophils primarily deal with parasitic infections and an increase in them may indicate such.
• They are also the predominant inflammatory cells in allergic reactions.
• The most important causes of eosinophilia include allergies such as asthma, hay fever, and hives; and also parasitic infections especially helminthic parasite.
• Basophils are chiefly responsible for allergic and antigen response by releasing the chemical histamine causing inflammation.
Monocyte.
• They have the kidney shaped nucleus and are typically agranulated.
• They also possess abundant cytoplasm.
• Monocytes share the ‘vacuum cleaner’ (phagocytosis) function of neutrophils, but are much longer lived as they have an additional role: they present pieces of pathogens to T cells so that the pathogens may be recognized again and killed, or so that an antibody response may be mounted.
They fight bacteria,fungi and viruses
• Monocytes eventually leave the bloodstream to become tissue macrophages which remove dead cell debris as well as attacking microorganisms.
• Neither of these can be dealt with effectively by the neutrophils.
• Unlike neutrophils, monocytes are able to replace their lysosomal contents and are thought to have a much longer active life.
Macrophage.
• Once monocytes move from the bloodstream out into the body tissues, they undergo changes (differentiate) allowing phagocytosis and are then known as macrophages.
Lymphocyte.
• Lymphocytes are much more common in the lymphatic system.
• Lymphocytes are distinguished by having a deeply staining nucleus which may be eccentric in location, and a relatively small amount of cytoplasm.
• The blood has three types of lymphocytes.
o B cells; which make antibodies that bind to pathogens to enable their destruction.o T cells; these include CD4+ (helper) T cells co-ordinate the immune response (they are what become defective in an HIV infection).o CD8+ (cytotoxic) are able to kill virus-infected and tumor cells.o T cells are crucial to the immune response because they possess a unique ‘memory‘ system which allows them to remember past invaders and prevent disease when a similar invader is encountered again.o Natural Killer Cells (NK cells).o Natural killer cells are able to kill cells of the body that are infected by a virus or have become cancerous.
Platelets.
• Platelets or thrombocytes are minute fragment of cells consisting of a small amount of cytoplasm surrounded by a plasma membrane.
• Platelets are roughly disk-shaped and an average about 3μm in diameter.
• They play an important role in controlling blood loss by forming platelets plugs which seal holes in small vessels.
• The life expectancy of platelets is about 5 – 9 days.
• Platelets arise in a unique manner by the shedding of thousands of cytoplasmic fragments from the tips of processes of megakaryocytes in the bone marrow.
• The first detectable cell of this line is the highly basophilic megakaryoblast, followed by a promegakaryocyte stage, in which synthesis of granules begins.
• Finally, the fully differentiated megakaryocyte, a giant cell with a large, dense, polyploid, multilobed nucleus, appears.
I just have to introduce this hacker that I have been working with him on getting my credit score been boosted across the Equifax, TransUnion and Experian report. He made a lot of good changes on my credit report by erasing all the past eviction, bad collections and DUI off my credit report history and also increased my FICO score above 876 across my three credit bureaus report you can contact him for all kind of hacks . Email him here support@wavedrive.tech go on their website wavedrive.tech for more details,Whatsapp No:+14106350697 if you want to chat them up,One thing i can assure you would not regret this at all he is 100% legit.